How Sharps and Needlestick Injuries Affect Medical Students
Sharps and needlestick injuries are a serious occupational health risk for those in the healthcare industry. This is especially true for medical students who still lack the clinical experience and expertise needed to properly handle and care for sharps. In addition to medical students, students studying biology and other sciences that use scalpels are at a risk as well.
Aside from the danger of injuries like nerve damage, exposure to sharps that have been potentially contaminated with Blood-Borne Infection (BBI) can lead to Hepatitis B (HBV), Hepatitis C (HCV) or Human Immunodeficiency Virus (HIV) infection.1
Those injuries represent undue burden costs not only to the students but also to the university. Most of the direct cost of treatment is shouldered by the college or university but follow up appointments and the treatment of side effects might not be supported.
As an example, in a study of post-exposure treatment of sharps injuries in Korea, health care workers that had a sharps injury has cost 34 local hospitals an estimated US $884,385 annually.2 That was mostly due to pharmacy, lab tests, and basic medical services. That cost still does not account for medical treatment in cases where the health care worker had contracted BBIs or if surgery is required to fix severed nerves or arteries.
Aside from the direct costs, hidden burdens exist for the medical student – such as delays in finishing the semester and the time to obtain the medical degree. These can result in significant duress and unneeded stress to the student and their families.
Although the risk of blood-borne infections from a single sharps injury is low, its consequences to an infected medical student can impact their long-term health as well as career-lasting impacts as it may restrict their career pathways.
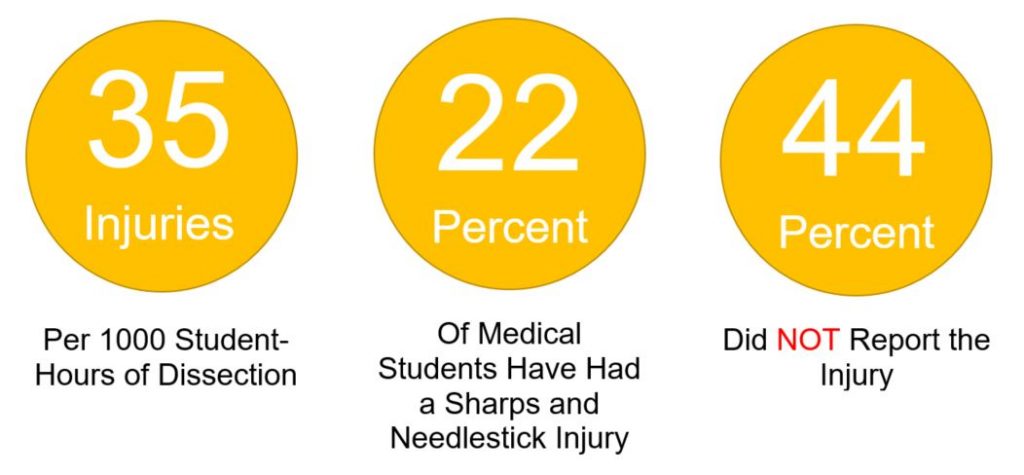
Some quick statistics on risks that medical students face:
According to a recent study conducted at the University of St Andrews Scotland UK over a 5-year period, for every 1000 hours of scalpel usage in a dissecting laboratory there were 35 injuries.3 Over a fifth of the medical student population have had a sharps or needlestick injury. And more worryingly, nearly half of the students did not report the incident.
In the same study the authors conclude that, “The following factors have contributed to increased safety influencing frequency rates: single-handed blade removal systems; mandatory personal protective equipment; and having only one student dissecting at a given time.”
It has been found out that using a single-handed blade remover with neutral zone was up to five times safer than a safety scalpel.4 Single handed blade removers like those pioneered by Qlicksmart can be seamlessly integrated into a university’s safety curriculum:
- Use of a scalpel blade removal system mounted in several stationary points within the laboratory increasing its accessibility scalpel blade removal can be completed at point of use
- The count is made easy with clear cartridges
- Automatic containment of used scalpel blades ensures that all students are protected from injury
By keeping them safe, medical students can focus on what’s important – learning. The right safety products can help them maintain a safe learning environment and help reduce the chance of experiencing a sharp injury. If students develop safety practices early in their careers, it might not only just save their future in the medical industry, but also their very own lives.
References:
- Rice, B., Tomkins, S. and Ncube, F. (2015). Sharp Truth: health care workers remain at risk of bloodborne infection. Occupational Medicine Advance Access. Oxford University
- Oh, Hyang Soon et al. (2012). Costs of postexposure management of occupational sharps injuries in health care workers in the Republic of Korea. American Journal of Infection Control, Volume 41, Issue 1, pp 61 – 65
- Foytl, J., Chisholm, F. and Varsou, O. (2019), Sharps injuries during dissection: a five‐year retrospective study in the context of safety. Anat Sci Educ. doi:10.1002/ase.1894
- Bit, A. (2018). Overview of surgical instruments for the operation theatre. Design and Development of Affordable Healthcare Technologies, pp 29.




good piece