How to Evaluate Safety Implementation in Healthcare
As we know, having a safety plan is extremely important in healthcare. Risks of injury can incur financial costs to a facility, and have physical and emotional effects on injured healthcare workers. For these reasons, it is important to be able to effectively implement safety plans and measures to mitigate identified risks to safety. The Centers for Disease Control (CDC), suggests regular risk assessment and reduction activities1. In previous blogs, Qlicksmart has looked at how facilities and people can invest in healthcare worker safety and how facilities can translate safety ideas into practice. But how do we know if changes to safety are being taken up by staff and safety is improving?
Evaluation is a very important part of safety implementation. Without this step of implementation, it can be difficult to know if changes are being engaged with by staff and effectively reducing risks to safety. As a part of implementing safety into practice, the National Health Service (NHS) in the UK has published a guide on Managing the Risks of Sharps Injuries2. It lists performance monitoring and review as the final step to implementing a safety plan. The guide recommends that “steps should be taken to periodically review the effectiveness of the risk assessment and control measures in place” (page 17). In the US, the Occupational Safety and Health Administration (OSHA) offers a Self Assessment Tool for hospitals to use. The questionnaire is designed to assist hospitals in evaluating their implementation of key safety and health management activities3 by monitoring employee participation (page 3 of assessment tool) and other factors.
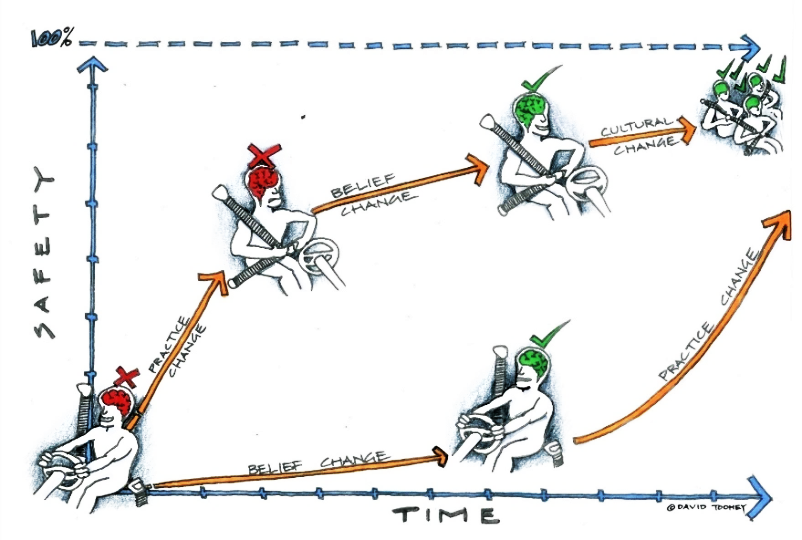
By evaluating safety participation among staff, changes and safety devices can be implemented more accurately. The infographic below uses seatbelts as an example to illustrate how evaluating change participation can optimise the implementation process to create a safer environment.
In a similar way, medical facilities can use tools like the Safety Score Card to measure staffs’ utilisation of sharps safety devices. Designed by Dr. Michael Sinnott, a notable expert in the field of sharps safety research, the safety score card calculates a “safety score” from 0.00 to 1.00 based on the facility’s purchasing data of devices being used with; no safety, active safety, and passive safety mechanisms. By using data from consecutive years or time frames, the score card can illustrate trends of safety device utilisation among staff. This allows a facility to see if the number of safety devices being used is increasing or decreasing.
By measuring utilisation, a facility can;
- Better understand clinicians’ engagement with sharps safety programs,
- More accurately standardise device purchasing,
- Perform audits and checks more precisely, and
- Reduce implementation costs where necessary.
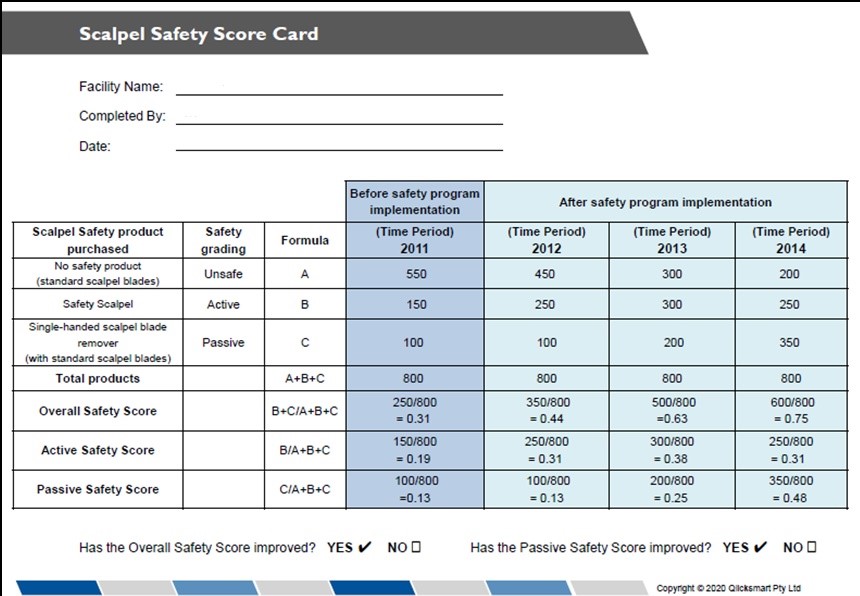
The safety score card makes up part of the Implementing Sharps Safety section of Qlicksmart’s Digital Platform. As the developers and manufacturers of safety medical devices that can reduce injuries such as the BladeFLASK, Qlicksmart has created the Digital Platform to guide users and facilities through the process of implementing safety.
You can download the safety score cards to start evaluating device usage in your facility at the links below:
References
- National Health Service (2015). Managing the Risks of Sharps Injuries. Nhsemployers.org. Retrieved 15 June 2020, from http://www.nhsemployers.org/-/media/Employers/Documents/Retain-and-improve/Health-and-wellbeing/Managing-the-risks-of-sharps-injuries-v7.pdf.
- Paschal, S. (2018). OSHA’s Injury & Illness Prevention Policy. Simon Paschal PLLC. Retrieved 15 June 2020, from http://simonpaschal.com/osha-injury-illness-prevention/.
- Centres for Disease Control and Prevention – Infection (2019). Risk Assessment | HCP | Infection Control Guidelines Library. Retrieved 15 June 2020, from http://www.cdc.gov/infectioncontrol/guidelines/healthcare-personnel/assessment.html.


