New Australia Standards AS 3825:2020 Procedures and Devices for the Removal, Containment and Disposal of Scalpel Blades
In December 2020 Standards Australia published AS 3825:2020 Procedures and devices for the removal, containment and disposal of scalpel blades from scalpel handles to replace the 1998 version, AS/NZS 3825:1998.
This revision enabled the inclusion of new information and the removal of one outdated section based on the latest published data to ensure optimal safety for all users of scalpel blades. Below I have done a comparison of the two Standards and included a link to purchase the new Standard.
AS 3825:2020 Standard compared to AS/NZS 3825:1998 Standard
There are several changes from the original 1998 Standard to this latest 2020 revised Standard. The following points outline the additions and differences:
Expanded Preface
-
- To include new users of scalpel blades, such as aesthetic clinics who use scalpels to perform dermaplaning and most importantly to highlight the three most important changes
-
- Expansion to include both multiple-use and single-use scalpel blade removers
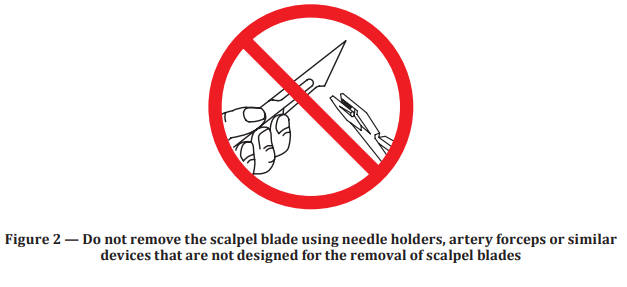
- Removal of unsafe practices such as using as using artery forceps to remove used scalpel blades, and
- Specification of the immediate containment of removed scalpel blades to provide protection against injury to downstream staff
-
- To include new users of scalpel blades, such as aesthetic clinics who use scalpels to perform dermaplaning and most importantly to highlight the three most important changes
-
- Definitions have been expanded to
-
- Include updated concepts about safety, namely “Passive” or Automatic/Single-handed safety devices and “Active” or manual safety devices. This is consistent with recent publications showing up to 70 times less injuries with Passive safety devices when compared to Active safety devices.
- Cover both single-use and multiple use blade removers with specific requirements for single-use devices which can be used in a sterile field, by including the terms “chamber” and “container”
- The addition these new terms, “chamber” and “container” also facilitates the requirement for a removed scalpel blade to be immediately contained. This adds protection from injury to both the user and downstream staff. Downstream staff include wardies/porters and staff working in the laundry. These people suffer between 6 and 10% of all sharps injuries.
-
- Definitions have been expanded to
-
- Design requirements for scalpel blade removal devices
-
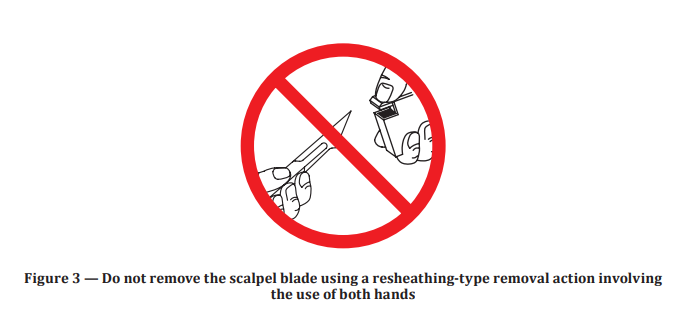
- Stipulates that the scalpel blade removal device can be used with a single-handed action
- That the safe removal is indicated with an audible sound and/or a visual cue
- That safe removal of the scalpel blade is immediately followed by containment of the removed blade
-
- Design requirements for scalpel blade removal devices
-
- Procedures for the removal of scalpel blades
-
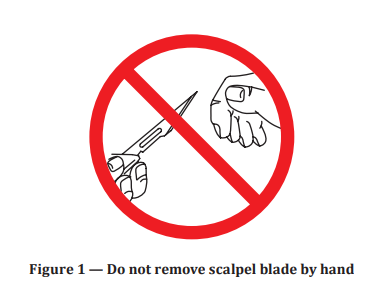
- The core features of using a scalpel blade remover (now stipulated to be operated single-handedly) and stopping the use of fingers or forceps (or other two handed devices) to remove used scalpel blades was maintained and strengthened.
-
- Procedures for the removal of scalpel blades
-
- The perceived weakness of the original Standard was that staff could use “un-safe” practices, namely using artery forceps to remove used scalpel blades if they were trained to do so, has been removed. Training people to complete un-safe practices was deemed counter intuitive and problematic.
- Procedures for the disposal of scalpel blade removers
-
- This is a new section. The original Standard only referred to disposal of the scalpel blade and not the actual scalpel blade removal device that contains the scalpel
-
- The perceived weakness of the original Standard was that staff could use “un-safe” practices, namely using artery forceps to remove used scalpel blades if they were trained to do so, has been removed. Training people to complete un-safe practices was deemed counter intuitive and problematic.
Five Additional Appendices
The original Standard referred to functional tests, such as the drop test, puncture test etc to those in the Sharps Container Standards. Drop test is now in Appendix B. The puncture test has been removed.
-
- Appendix A and B are normative. Appendices C, D and E are informative.
- Appendix A
-
- Specifies how a scalpel blade removal device should be tested for both its ability to safely removal and immediately contain the removed blade
- It specifies testing for both single-use and multiple-use scalpel blades
- Noteworthy is the addition of protection of operators in independent labs carrying out assessment of scalpel blade removers with the inclusion of a recommendation that they use blunt scalpel blades or cut-resistant gloves
-
-
- Appendix B
-
- Specifies how the “drop test” is to be performed for both single-use and multiple-use scalpel blade removers
-
- Appendix B
-
- Appendix C
-
- Provides a template for recording and reporting the findings on inspection of features such as the audible or visible cue is included for use with Appendix A
-
- Appendix C
-
- Appendix D
-
- Covers both initial training and a periodic review of competency
-
- Appendix D
-
- Appendix E
-
- Includes audit of both the compliance of and the number of scalpel blade removal devices.
-
- Appendix E
The new AS 3825:2020 Standard will assist all users of scalpel blades to better protect themselves and their staff from preventable scalpel blade injuries. Main topics that were added include training people to use single-handed blade removers and procedures for the disposal of scalpel blade removers.
Name Change
The original 1998 Standard was a joint effort between the Australian and New Zealand Standards organisations. In 2016 however, Standards New Zealand underwent a number of changes and subsequently became part of the New Zealand Government. As such, it no longer routinely collaborates with Standards Australia. Due to this a revision to the original Standard has been done by Standards Australia alone. This explains the new reference number and title – AS 3825:2020 Procedures and devices for the removal, containment, and disposal of scalpel blades from scalpel handles.
Qlicksmart single-handed blades remover
Qlicksmart single-handed blades removers eliminate the dangers of removing scalpel blades with safe removal and containment of used blades. These devices can be seamlessly integrated into current practice. The surgeon continues to use his/her preferred traditional metal handle and the nurse uses this single-handed safety device to remove the used scalpel blade (instead of fingers or forceps). Automatic containment of the used scalpel blade also ensures that downstream staff are protected from injury.
- BladeFLASK is the world’s first single-handed, passive safety scalpel blade remover and acts as a single-use sharps container in its own right. It accommodates up to 100 blades and incorporates an automatic shut-off to prevent over-filling.
- BladeFlaskEVO is the latest innovation from Qlicksmart. It can accommodate even more types of BP scalpel handles and blades including large autopsy scalpels, thick and round handles, even hexagonal shaped versions – giving you greater freedom in using any scalpel you want.
- BladeCASSETTE is designed to allow the single-handed removal and safe containment of up to 3 used blades in the sterile field. It can also be incorporated into custom procedure packs.
- BladeSINGLE is designed to allow the single-handed removal and safe containment of 1 used blade in the sterile field. It can also be incorporated into custom procedure packs.
- BladeNeedleSYSTEM is a dual-purpose safety device incorporating a Needle Counter (20 count) and single-handed blade removal and containment of 2 used blades. Extra Qlicksmart removal cartridges can be added to the device if required.
If you have any questions regarding the new Standard regarding the Procedures and devices for the removal, containment, and disposal of scalpel blades from scalpel handles, please contact us at hello@qlicksmart.com.
The Australian Standard can be purchased from Standards Australia – http://www.standards.org.au/standards-catalogue/sa-snz/health/he-011/as–3825-colon-2020.
Dr. Michael Sinnott, MBBS, FACEM, FRACP, has contributed to over 40 publications and is a world-leader in research regarding staff safety in healthcare, particularly scalpel safety. His expertise in staff safety lead Dr Sinnott to become involved in the development of safety guidelines and legislation in the USA, and safety standards in Australia. As part of his advocacy for staff safety, Dr Sinnott Co-Founded Staff and Patient Safety, a not-for-profit organisation which provides a platform for staff and patient safety issues. In the field of research, Dr Sinnott promotes an evidence-based approach to emergency medicine research and practice, and the development of a culture which generates and supports research findings. Dr Sinnott was a driving force in designing the Queensland Emergency Medicine Research Foundation, which has raised over $26 million dollars for Queensland Emergency Medicine research teams.
References
- Procedures and devices for the removal, containment and disposal of scalpel blades from scalpel handles. AS 3825:2020 Standards Australia
- Safety-engineered needle devices: evaluation prior to introduction is essential. Adams, D. et al. Journal of Hospital Infection, Volume 79, Issue 2, 174 – 175