Skin Deep – Sharps Cuts in Dermatology
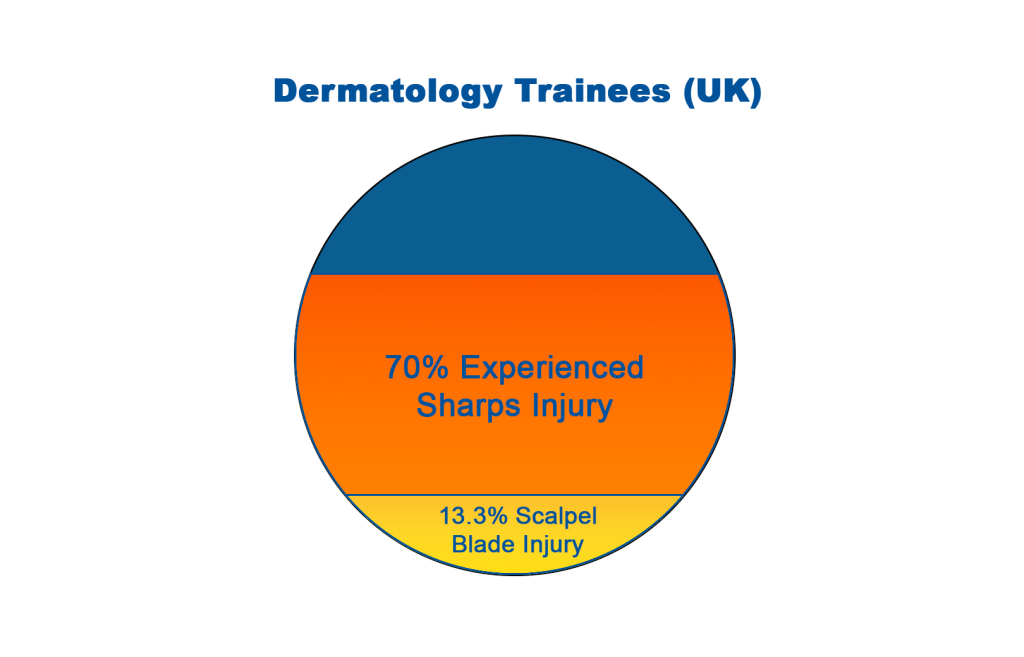
As dermatologists are often required to do operative procedures, sharps injuries occur and can have significant consequences.
Sharps Injuries in Dermatology
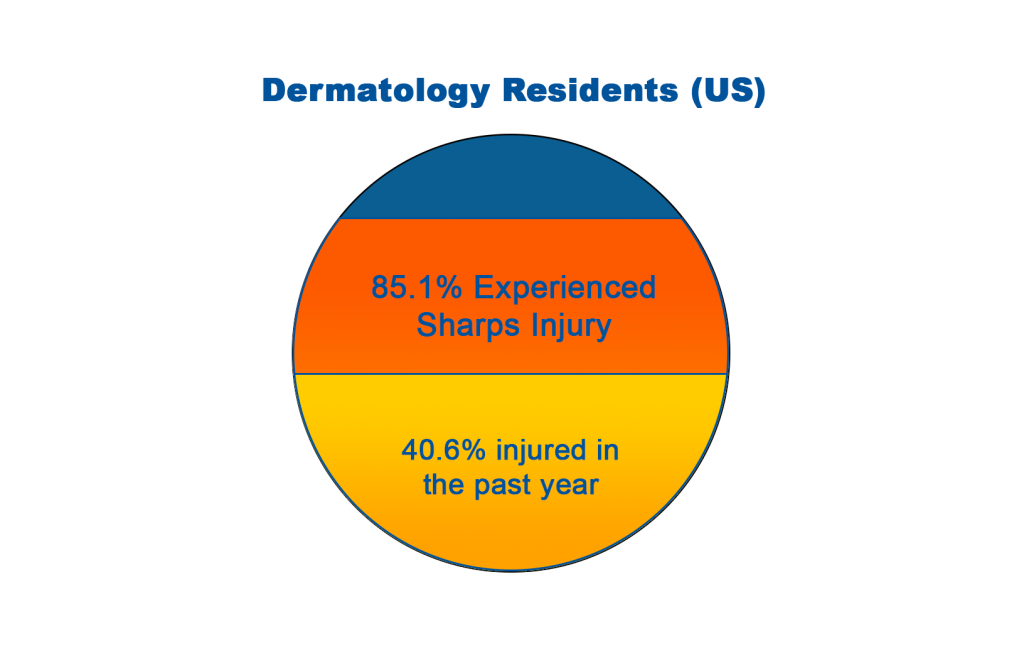
Similarly, 85.1% of dermatology residents in a study from the United States reported having experienced a sharps injury; 40.6% of these injuries had occurred within the previous year.
The results further states, “Sixty-eight injuries occurred during surgery (58.6%), and 106 were perceived to be self-inflicted (91.4%). Physicians most likely to report recent sharps injuries were trainees (26/41, 63.4%), dermatologic surgeons (24/64, 37.5%), and medical dermatologists (3/11, 27.3%). One hundred eighty-three (64%) respondents reported having ever had a sharps injury that went unreported.”
The authors of the study concluded, “Sharps injuries are common among dermatologists. Underreporting is common and places providers and patients at risk of blood-borne illnesses.”
Preventing Sharps Injuries in Dermatology
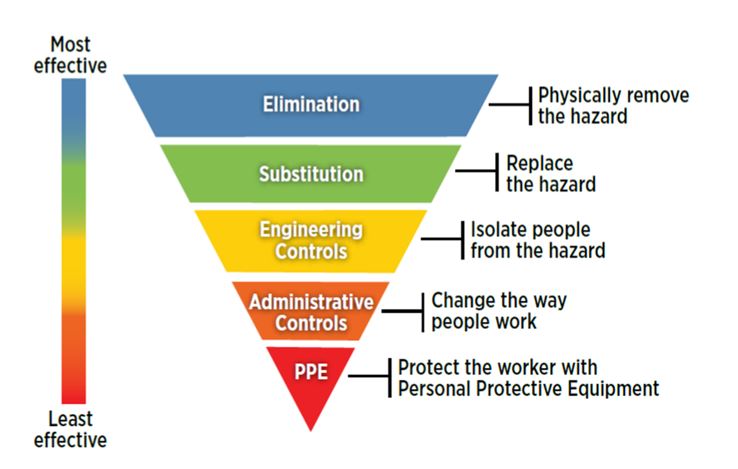
An effective way to reduce the likelihood of sharps injuries occurring among dermatology practitioners is by implementing the Hierarchy of Controls. The Hierarchy of Controls was created by the National Institute for Occupational Safety and Health (NIOSH) in the United States and has been integrated into workplace health and safety laws and regulations across the world. It outlines five methods of hazard control, which are prioritised in order of their effectiveness:
Although most effective, elimination and substitution is not always feasible. In dermatology specifically, sharp instruments such as scalpels are necessary to make incisions needed for removal and treatment of various skin conditions. Hospitals, healthcare facilities, and clinics such as dermatology practitioners should offer safety-engineered equipment as part of Engineering Controls in the Hierarchy of Controls to stop the rising rate of sharps injuries.
Engineering Controls against sharps injuries include safety-engineered devices such as scalpel blade removers and spring-loaded safety syringes. A scalpel blade remover which contains the used scalpel blade also protects downstream staff like cleaners from injuries. It’s also important that staff are trained in how to correctly use the safety device and all sharps control measures in place.
Specifically, engineering controls incorporate safety mechanisms designed to either isolate or remove the hazard from the environment.
The Occupational Safety and Health Administration (OSHA) in the US requires facilities to ensure the following:
-
- Engineering and work practice controls shall be used to eliminate or minimize employee exposure. Where occupational exposure remains after institution of these controls, personal protective equipment shall also be used.
- Engineering controls shall be examined and maintained or replaced on a regular schedule to ensure their effectiveness.
- Annual training for all employees shall be provided within one year of their previous training.
Qlicksmart Safety-Engineered Devices
Qlicksmart’s BladeFlask EVO multi-use scalpel blade remover is compliant with sharps safety guidelines for the medical industry. The BladeFlask EVO is a safety device optimised for dermatology clinics because it:
-
- Is compatible with all BP handles including the bulbous, thick, and ergonomic handles.
- Is compatible all BP scalpel blades including large blades that are often used in dermatology
- Is safe and easy to use with a single-handed operation
- Can be wall, bench or trolley mounted using the Qlicksmart universal Mounting Bracket, allowing for blade removal at point of use
- Is compliant with UN Transport Requirements of Dangerous Goods (for sharps waste) and can be disposed as a sharps container
With little to no training required, Qlicksmart’s single handed blade removers are proven to reliably reduce the risk of scalpel cuts and injuries. If you’d like to make your practice safe from scalpel injuries, don’t hesitate to contact us at hello@qlicksmart.com.
References
1. A. Kelly, R. Gandhi and J. Natkunarajah, DS17: A pilot survey of sharps injuries among dermatology trainees in London centres. Br J Dermatol 2021, 185: 110-111. https://doi.org/10.1111/bjd.20240
2. Donnelly, Abigail F. MD1; Chang, Yu-Hui H. PhD2; Nemeth-Ochoa, Shari A. MD1. Sharps Injuries and Reporting Practices of U.S. Dermatologists. Dermatologic Surgery: December 2013 – Volume 39 – Issue 12 – p 1813-1821 https://doi.org/10.1111/dsu.12352