Under-reporting scalpel injuries: the risks to healthcare staff and institutions
In 2008, a survey by the Royal College of Nursing found that while 50% of nurses had sustained a sharps injury, only 10% of those injuries were reported. This means that even in dangerous situations where there are safety risks, approximately 90% of sharps injuries are not reported. A sharps injury such as a scalpel injury can create countless issues for the victim including lacerations, blood-borne disease, and more. Furthermore, under-reporting scalpel injuries hinders an institution’s ability to respond to workplace hazards. So why aren’t staff members speaking up and reporting these injuries when they pose such a huge risk?
What a scalpel injury means for the victim
Severing digital arteries nerves and tendons, mental health issues, and contracting blood-borne disease are all very real consequences of a scalpel injury. The top three blood borne diseases contracted from scalpel injuries are Hepatitis B, Hepatitis C, and HIV. Waiting months for blood test results, can be a nerve-wracking, anxiety-inducing experience. The anxiety surrounding a sharps injury and potential loss of income can directly affect those in close contact with a victim too – especially if the victim supports a household. Moreover, single scalpel injuries have been known to cost medical institutions valuable staff, and up to millions of US dollars in treatment and ongoing costs. Evidently, if a scalpel injury is not correctly reported and treated, it can change and even threaten a person’s life.
Why are people under-reporting scalpel injuries?
Staying silent about scalpel injuries can often be seen as the easier option. A qualitative study in the US found the top three reasons healthcare staff don’t speak up about safety risks are: fear of being viewed negatively, feeling as if they don’t have enough experience or tenure, and perceiving their organisation’s structure to be intimidating and/or unsupportive. Another influential reason cited for not reporting scalpel injuries is the fear of confirming a blood-borne infection.

The benefits of reporting scalpel injuries
Reporting an incident not only helps staff members or patients that may be at risk, but it also allows healthcare institutions to detect, correct, and prevent unsafe work practices and complications. Under-reporting scalpel injuries can seriously hinder an institution’s ability to respond to safety concerns. Employee’s psychological safety, teamwork and culture among units, staff turnover, and patient safety are just some of the things that Under-reporting can cause issues for.
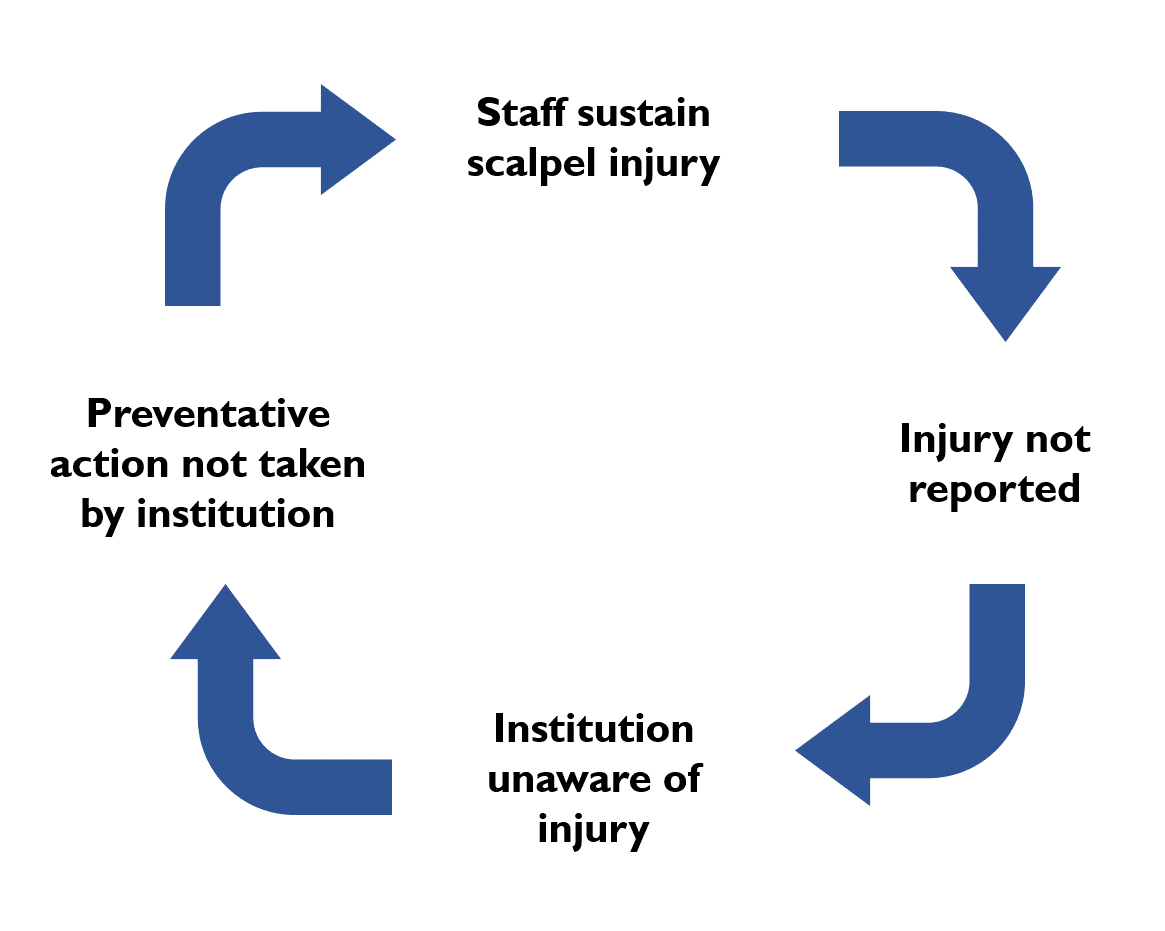
The below diagram shows the vicious cycle that not reporting a scalpel injury creates. If an injury is not reported, the institution cannot take preventative action such as reviewing their sharps policy procedures to make sure the injury doesn’t happen again. When the injury does happen again the cycle repeats itself.
How to adequately respond to scalpel injury concerns
With increased reporting, an institution would be notified about breaches of safety and can then introduce preventative measures through a sharps policy program. There are a number of ways a sharps policy program can help healthcare institutions reduce scalpel injuries. An effective sharps policy program for example, should include a reporting system that encourages and supports staff, and identifying preventative measures to avoid scalpel injuries. Combining the use of a hands-free passing technique (HFPT) and a single-handed scalpel blade remover, for example, is arguably the most effective method and can reduce scalpel blade injuries by up to 50%.
Ultimately, it is up to both the institutions and staff to improve safety. By encouraging the reporting of scalpel injuries and adequately addressing them through sharps policy programs, healthcare institutions can create a positive safety culture where healthcare workers can safely focus on caring for patients. Similarly, by reporting injuries staff will not only make it easier for institutions to respond to issues, but they will also create a positive culture focused on safety.
Reference List
Trim JC, Elliott TSJ. A review of sharps injuries and preventative strategies. Journal of Hospital Infection 2003;53(4):237-42. doi: 10.1053/jhin.2002.1378
AfPP. Sharps Injuries in the Operating Theatre – A Practical Guide to Further Reducing the Risks: Purple Sugical 2015.
Hoffmann C, Buchholz L, Schnitzler P. Reduction of needlestick injuries in healthcare personnel at a university hospital using safety devices. Journal of occupational medicine and toxicology (London, England) 2013;8(1):20-20. doi: 10.1186/1745-6673-8-20
Saia M, Hofmann F, Sharman J, et al. Needlestick injuries: incidence and cost in the United States, United Kingdom, Germany, France, Italy, and Spain. Biomedicine International 2010;1(2):419.
Adams D, Elliott TSJ. Safety-engineered needle devices: evaluation prior to introduction is essential. Journal of Hospital Infection 2011;79(2):174-75. doi: http://doi.org/10.1016/j.jhin.2011.05.020

