What Goes Unreported Goes Unfixed: Why Are Sharps Injuries Still Going Unreported in the OR?
The reporting of injuries, errors and near misses is important for both staff and patient safety. Think about the last time you had, or you saw or heard about an injury at work. Did you report it or check whether this injury was reported?
Case Study
A 44 year old pathologist suffered what he dismissed as a minor scalpel cut during a routine post-mortem examination. He stabbed the dorsum of his left thumb over the interphalangeal joint. He immediately irrigated it but then chose to ignore it – both clinically and from a reporting perspective
After a delay of 16 hours, he felt a bit feverish and decided to present to ED.
He was a healthy non-smoker, on no medications. In the ED he was afebrile and a 5mm laceration was noted with a distal haemorrhagic blister. There was no pain and ROM was full.
He was given empiric antibiotics. The wound was incised and drained. The ED staff were concerned and elected to observe him for a bit longer.
2 hours later he was still afebrile, but his HR had risen to 130 and his WCC came back at 20.
This rapid deterioration, now 18 hours after the injury, saw him taken to operating theatre for debridement with the diagnosis of necrotizing fasciitis.
Public Citizen Report
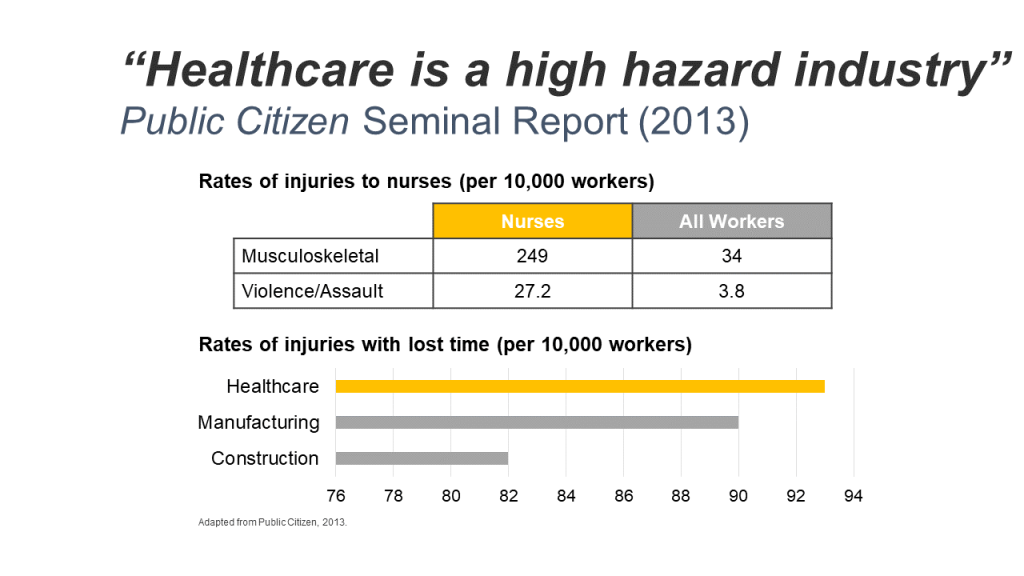
In 2013, the Public Citizen, a not-for-profit organization, published its seminal report, in which they concluded that healthcare is a high-hazard workplace.
They found that in the US, there were 7 times as many musculoskeletal injuries in healthcare than in manufacturing and construction industries. In the same report, they also mentioned that there were 7 times more assaults in healthcare than in manufacturing and constructions industries.
We have to stop thinking it is just a normal part of the job – something that you have to put up with.
Sharps Injuries
The incidence of sharps injuries is continuing to rise in the operating rooms. 10 years after the Needlestick Safety and Prevention Act was passed in the USA, sharps injuries in non-surgical settings fell by 31.6%.
However the data showed that there was no similar decrease in injuries in the operating room. In fact, there was a 6.5% increase, with most of the injuries caused by suture needles and scalpel cuts.
Whilst there was so much focus on needlestick injuries, injuries from other sharps such as scalpel blades were overlooked, resulting in them being referred to as the forgotten sharps injuries.
How Many Injuries are Going Unreported?
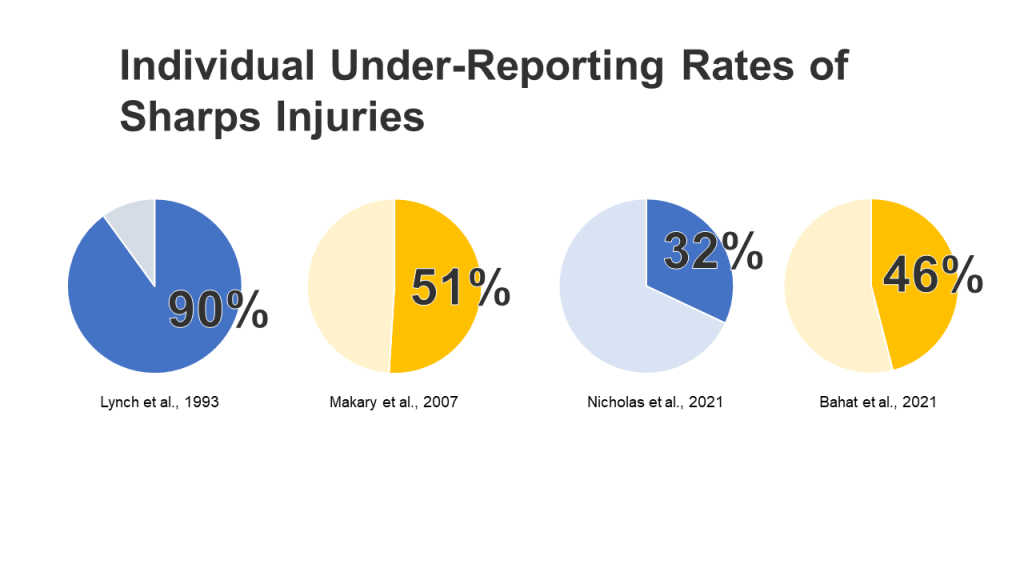
Looking specifically at under-reporting for sharps injuries, we’ve had to put up international statistics, as there is currently no routine national surveillance of sharps injuries in Canada. Researchers in Canada have noted that this lack of national data has made it difficult to both identify the risks to healthcare workers, and the impact of safety interventions if and when they are introduced.
In the United States, education and awareness would appear to be having some effect in reducing under-reporting rates of sharps injuries. As you can see back in 1993, individual underreporting rates were found to be 90%, improving to 50% by 2007. This is likely, in part, due to US legislation and regulations which have stricter reporting requirements for bloodborne pathogen exposures due to splashes and sharps injuries. Two studies published in 2021 show an average of around 40% of all sharps injuries are still being under-reported despite these mandates.
Even more relevant for today is that 2 of these 4 studies also found that underreporting was highest in the OR.
Why Are We Under-Reporting?
Denial
Self Blame Culture
Why Are We Under-Reporting: Organisational Factors
- Perception that nothing gets done
In 2018, The Joint Commission in the USA published the Sentinel Event Alert # 60. In this alert they shared that every year the Joint Commission receives reports from healthcare staff about unsafe conditions in their organizations. The Joint Commission said that the majority of these reports indicated that leadership had not been responsive to these reports from staff and other early warnings, even though their response may have prevented harm events from occurring.
- Why Are We Under-Reporting: Fear of punishment
In a Canadian university hospital, healthcare workers speaking up about patient and staff safety issues were labelled as “troublemakers” and faced discipline. They were threatened against talking publicly and faced discipline within their workspaces. These incidents created a culture of fear where safety concerns were not always reported, as clinicians thought it would put their own jobs on the line. However. brave nurses and clinicians did speak to CTV News Vancouver to try to bring attention to these bad conditions for staff and patients, but had to do so anonymously.
Unreported Injury Impact: The Injured Healthcare Worker
-
- Physical injury may become more complicated (e.g. Pathologist case study)
- Guilt and shame follows injury and goes unchecked.
- Psychological injury does not get treated.
Unreported Injury Impact: The Clinical Team
-
- Team morale decreases when injuries occur.
- Team is at risk of repeated injuries.
- Teams need support from each other for future protection.
Unreported Injury Impact: The Patients
According to OSHA:
- Patient and worker safety often go hand-in-hand.
- Efforts to reduce the rate of medical error must be linked with efforts to prevent work-related injury and illness if they are to be successful.
According to the World Health Organization:
- No country, hospital or clinic can keep its patients safe unless it keeps its health workers safe.
- Protecting health workers is key to ensuring a functioning health system.
Unreported Injury Impact: The Facility
As a result of underreporting, is facilities miss the opportunity to invest in prevention and save money in the medium and long term. Injuries can’t be examined with a view to developing products and evidence-based strategies to prevent these injuries recurring.
What Can We Do To Increase Reporting Rates?
-
- Audit Current Practices
- Improve Reporting System
- Improve Root Cause Analysis
- Improve Training Programs
- Improve Collaborative Communication
- Run “Good Catch Campaigns”
- Prioritise Staff Safety
Connecting the Dots
| Actions taken: | Will help prevent: |
| Audit Current Practices | Denial |
| Improve Reporting System | Reporting Systems being Time Consuming & Confusing |
| Improve Root Cause Analysis | Surface-Level Root Cause Analysis
Perception that Nothing Gets Done |
| Improve Training Programs | Denial
Unnecessary Self-Sacrifice |
| Improve Collaborative Communication | Self-blame
Fear of Punishment |
| Run “Good Catch” Campaigns | Self-blame
Perception that Nothing Gets Done |
| Prioritise Staff Safety | ALL CAUSES OF UNDER-REPORTING |
Summary
By understanding and addressing the impediments to staff reporting their concerns, reporting rates can be improved.
Once accurate and complete reporting data is available, it can be analysed and used to design prevention strategies.
Prevention strategies need to be implemented in a systematic way using the Hierarchy of controls.
Finally, that reported data can be used in audits to ensure that the achieved improvements in safety are maintained and embedded in the hospitals culture.
Reference
- Bahat, H., Hasidov-Gafni, A., Youngster I., Goldman, M., & Levtzion-Korach, O. (2021). The prevalence and underreporting of needlestick injuries among hospital workers: a cross-sectional study. International Journal for Quality in Health Care, 33(1), 1—5. https://doi.org/10.1093/intqhc/mzab009
- Brichacek, M., Strazar, R., Murray, K. & Islur, A. (2017). Necrotizing fasciitis after scalpel injury sustained during postmortem examination. CMAJ, 189(20), 721– E723
- Boden, L.I., Petrofsky, Y.V., Hopcia, K., Wagner G.F., & Hashimoto, D. (2015). Understanding the hospital sharps injury reporting pathway. American Journal of Industrial Medicine, 58, 282—289. https://doi.org/10.1002/ajim.22392
- Daflos, P. (2023, Jan 19). Threats, discipline, fear: The muzzling of B.C. health-care workers. CTV News Vancouver. https://bc.ctvnews.ca/threats-discipline-fear-the-muzzling-of-b-c-health-care-workers-1.6236966
- Daflos, P. (2023, Feb 9). Resignations and retaliation: B.C. health-care workers see increasingly ‘toxic’ workplaces. CTV News Vancouver. https://bc.ctvnews.ca/resignations-and-retaliation-b-c-health-care-workers-see-increasingly-toxic-workplaces-1.6265688
- Hambridge, K., Endacott, R., & Nichols, A. (2021). The experience and psychological impact of a sharps injury on a nursing student population in the UK. British Journal of Nursing, 30(15). https://doi.org/10.12968/bjon.2021.30.15.910
- Haskins, J. (2019, June 6). 20 years of patient safety. AAMC News. https://www.aamc.org/news-insights/20-years-patient-safety
- International Safety Center. (2019). OR Needlestick & Sharp Object Injury Report. https://internationalsafetycenter.org/wp-content/uploads/2018/12/EPINet-OR-2019-US-Needlestick-Sharp-Object-Injury.pdf
- Jagger, J. et al. (2011). ‘Increase in Sharps Injuries in Surgical Settings Versus Nonsurgical Settings After Passage of National Needlestick Legislation’. AORN Journal, 93(3), 322—330.
- Jump, J., Coogle, C.J. (2022). Redesigning the Perioperative Huddle to Improve Culture. AORN Journal, 115(4), 337—340. http://doi.org/10.1002/aorn.13641
- Lozito, M., Whiteman, K., Swanson-Biearman, B., Barkhymer, M., & Stephens, K. (2018). Good Catch Campaign: Improving the Perioperative Culture of Safety. AORN Journal, 197(6), 705—714. http://doi.org/10.1002/aorn.12148
- Makary, M. A., Al-Attar, A., Holzmueller, C. G., Sexton, J. B., Syin, D., Gilson, M. M., Sulkowski, M. S., & Pronovost, P. J. (2007). Needlestick injuries among surgeons in training. The New England Journal of Medicine, 356(26), 2693–2699.
- Nicholas, J., Grimmond, T., Bradywood, A., Church, E., Moran, J., & Ogg, M. (2021). AORN Journal, 114(4), 368—375. https://doi.org/10.1002/aorn.13502
- Public Citizen. (2013). Health Care Workers Unprotected – Insufficient Inspections and Standards Leave Safety Risks Unaddressed. https://www.citizen.org/wp-content/uploads/health-care-workers-unprotected-2013-report.pdf
- Sikorski, J. (2009). Connecting Worker Safety to Patient Safety: A New Imperative for Health-Care Leaders. Ivy Business Journal. https://iveybusinessjournal.com/publication/connecting-worker-safety-to-patient-safety-a-new-imperative-for-health-care-leaders/
- Sinnott M, Shaban, Smalley P R London M and Eley RM. (2013, March 2-7). Staff Safety – Why do we ignore it at our own Peril?: Scores to improve compliance with staff safety guidelines. AORN Global Surgical Conference 2013, San Diego.
- Tabachnick, D.L., Pena, J.P., Nabeel, I., & Klingman, K.J. (2021). Understanding Causes of Needlestick and Other Sharps Injuries Among OR Personnel. AORN Journal, 114(4), 361-367. http://doi.org/10.1002/aorn.13499
- The Joint Commission. (2018). Developing a reporting culture: Learning from close calls and hazardous conditions. Sentinel Event Alert, 60, 1-8.
- The National Steering Committee on Patient Safety. (2002). Building a Safer System: A National Integrated Strategy for Improving Patient Safety in Canadian Health Care. https://doi.org/10.7939/r3-yq69-gp38
- S. Bureau of Labor Statistics. (2022). Graphics for Economic News Releases: Number and rate of nonfatal work injuries and illnesses in private industries. United States Department of Labor. https://www.bls.gov/charts/injuries-and-illnesses/number-and-rate-of-nonfatal-work-injuries-and-illnesses-by-industry.html